Skin Cancer & Mohs
The most advanced treatment for skin cancer
Trust your surgery to a fellowship trained Mohs Surgeon.
Mohs Surgery is a specialized procedure for removing skin cancers, especially those that may be in cosmetically sensitive locations, have aggressive growth features, are recurrent, large, or in sensitive areas, such as the face or eyelid. Dr. David Kent and Dr. Steven Kent of Skin Care Physicians of Georgia are board-certified dermatologists who have completed specialized training with a year’s fellowship to perform this type of surgery.

“Performing Mohs Surgery allows me the honor to solve my patient’s skin cancer problems, while also focusing on their comfort, safety, and delivering excellent results.”
David E. Kent, MD

“Performing Mohs Micrographic surgery affords me the privilege of providing the highest level of care in treating patient’s skin cancers, delivering outcomes of the highest standard.”
Steven Kent, MD
Diagnosis of Skin Cancer
Types of Skin Cancer
One in five Americans will develop some type of skin cancer over the course of their lifetime. With early detection and treatment, however, most skin cancers are completely curable. Early detection and treatment of any form of skin cancer are essential both to prevent the disease from spreading to other areas of the body and to achieve better outcomes.
Basal cell carcinoma – This is the most common form of skin cancer, with more than 4 million new cases each year in the U.S.
It is usually caused by sun exposure and doesn’t normally spread to other parts of the body. They tend to grow very slowly and occur most often in sun-exposed locations. Often a patient may notice a growth that may be waxy or have a pearly appearance, with a rolled border. Often patients will notice a growth will crust over, heal, then crust and scab again. This is a common history for patients that present for evaluation with a basal cell carcinoma. Fortunately, basal cell carcinomas are almost always successfully treated based on the specifics of a patient’s problem.
Melanoma is a specific type of skin cancer that begins with the cells that produce pigment. Melanoma can occur on any skin surface and rarely in the eye.
The clinical signs of identifying melanoma are detected by simply using your “ABC’s” as follows:
ABC’s of Melanoma
The ABC’s of melanoma can help you to determine is a mole is possibly problematic.
- Asymmetry – Cancerous moles tend to be asymmetrical where one half does not look like the other.
- Border – benign moles have a smooth oval, round edges while melanomas often have irregular, jagged edges
- Color – benign moles tend to be a uniform color of brown or tan whereas cancerous moles are often irregular in color: black, brown, red, and the color can appear irregular.
- Diameter – benign moles generally are smaller than 6 mm which is the diameter of most pencils, whereas melanomas are often larger. Also, D can stand for darkness- if a mole is jet black in color.
- Evolution – benign moles typically don’t change in appearance whereas melanomas may change in appearance in any or all of the ABCD features above.
So, if you have a mole with any of the ABCDE findings that are described above, it is super important to call and have your mole evaluated by one of our skin experts to see if it may need a biopsy to confirm the diagnosis.
Treatment of Skin Cancer
Fortunately, the overwhelming majority of skin cancers are successfully treated in the office by one of several methods. The treatment options for a particular skin cancer are reviewed with each patient and a treatment plan is individualized. These options range from using a topical medicine for tiny very superficial lesions, to various surgical options.
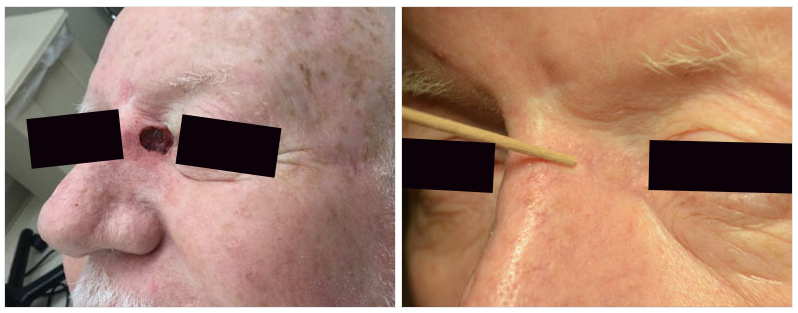
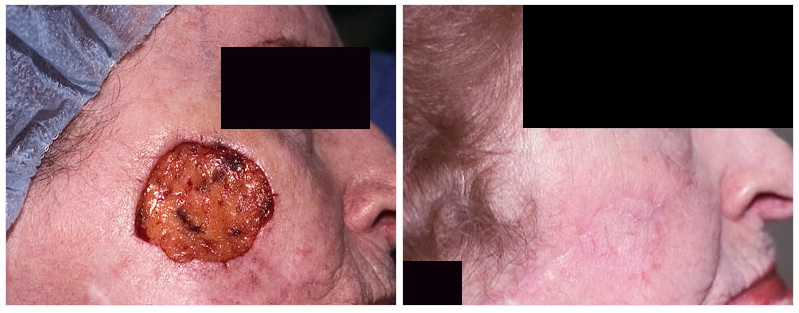
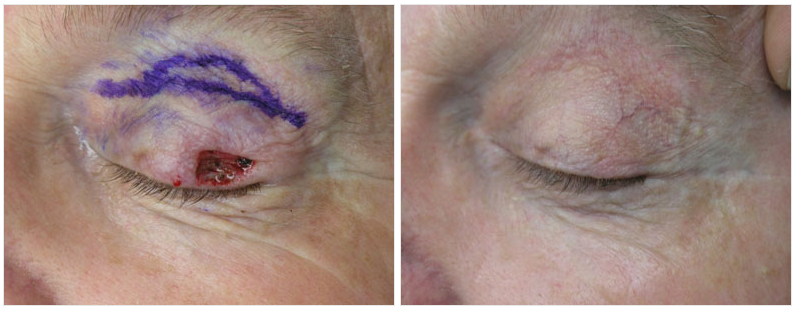
Mohs surgery is a highly specialized surgery for removing skin cancers especially those that may be located in cosmetically sensitive locations, have aggressive growth features, may be recurrent (removed and come back), be large, or in sensitive locations such as the face or eyelid.
SCPOG has two board-certified dermatologists who have completed specialized training with a year fellowship, (Dr. David Kent and Dr. Steven Kent). To learn more about Mohs surgery and why you should consider Skin Care Physicians of Georgia for treating your skin cancer and Mohs surgery click here.
Superficial Radiation Treatment (SRT): SCPOG is fortunate to have the only SRT unit in middle Georgia. It is a type of radiation treatment specifically designed for treating certain superficial skin cancers in sensitive areas without surgery in particular the central face and lower extremity. No downtime is necessary and the series of treatments is set up and each visit takes just a few minutes.
The lesion is removed with an adequate safety margin surgically and stitches are placed to allow for proper healing.
ED&C is simple scraping and cauterizing which is usually done in areas that are not cosmetically sensitive.
Why choose SCPOG for your Mohs Surgery?
- Certified by the American Board of Dermatology, member of the American College of Mohs Surgery
- 1st full time fellowship trained physician for Mohs Surgery outside of Atlanta in the state of Georgia since 1987
- Personally performed over 41,000 Mohs cases
- Expert in management of difficult and recurrent skin cancers
- Surgical staff at major hospitals in Macon with OR privileges
- Compassionate, caring, committed to patient comfort, safety, and results
- One of a small select group of physicians in the US with a nationally accredited training program who trains physicians to be experts in Mohs surgery and reconstruction
- We have two fellowship-trained Mohs surgeons in practice
- Dr. Kent has served as a faculty member for over 30 years at the Superficial Anatomy and Cutaneous Surgery course at UCSD and Scripps Clinic in La Jolla, California. Clinical faculty member of two medical schools: Medical College of Georgia and Mercer Medical School. Engaged in active training of medical students, physicians in training, as well as physician assistants and nurse practitioners. He has published numerous papers in peer reviewed journals on various topics including facial reconstruction following skin cancer removal.
Skin Care Physicians of Georgia specializes in evaluating and treating difficult and recurrent skin cancers. Dr. Kent has performed over 41,000 Mohs surgery cases over the past 34 years. For advanced and complex cases that may require anesthesia, Dr. Kent has OR privileges at the major hospitals in Macon, and if necessary, present cases for discussion at multidisciplinary tumor conferences.
For more detailed information about skin cancer, visit https://www.skincancer.org/skin-cancer-information/skin-cancer-facts/
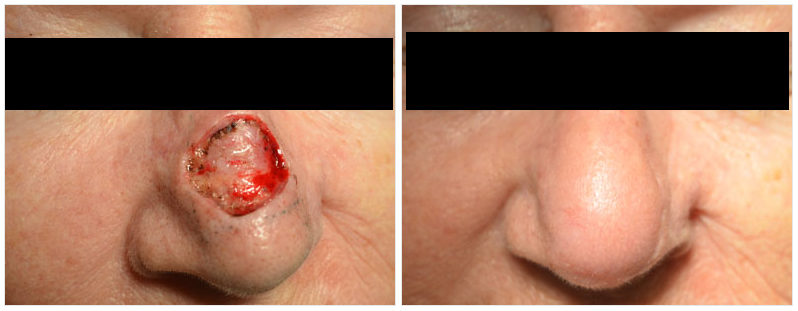
Before & After Gallery








SCHEDULE YOUR CONSULTATION*
*All consults are subject to a fee.